Antigen-Specific T Cells to Carcinoembryonic Antigen (CEA)
Our scientists were among the first to develop custom antigen-specific T cells for research use and have created them against a diverse range of targets, including viral, tumor, and self-antigens.
We’re now developing the next generation of antigen-specific T cells to target some of today’s most prevalent and challenging diseases. More on that below. But first, a primer on antigen-specific T cells.
The Role of Antigen-Specific T Cells in Disease Research and Treatment
T cells are a major player in the immune response in various diseases, including cancer and pathogenic infections, and are mediators in inflammation and autoimmunity. A large body of research has been conducted over the past few decades to manipulate T cell responses, leading to many clinical strategies including cancer vaccines, T cell adoptive therapy, CAR-T therapy, immune-oncology, and the use of regulatory T cells for autoimmune diseases.
Antigen-specific T cells are an important tool in T cell biology research and potency assays. Investigators can isolate them directly from the disease site (e.g., tumor-infiltrating lymphocytes (TIL) or inflammatory lesion infiltrate populations), but these procedures often yield a limited number of cells due to low cell frequency and lack of robust isolation methods.
Alternatively, antigen-specific T cells can be generated in vitro using antigen-presenting cells pulsed with whole antigens or peptides. However, this process is often time-consuming with a low success rate.
About Ignyte Bio’s Antigen-Specific T Cells
Ignyte Bio offers antigen-specific T cells for research use you can rely on.
- Typically generated using multiple in vitro stimulations with peptide antigens
- Not immortalized or genetically modified, so they more closely mimic physiological T cells
- Specificity analyzed using the cognate peptide/MHC tetramer binding as well as interferon-gamma (IFN-γ) secretion assays.
Announcing Ignyte Bio’s Newest Antigen-Specific T Cells : anti-CEA CD8+ T Cells
Carcinoembryonic antigen (CEA) is a 180-kDA cell surface glycoprotein overexpressed in 90% of gastrointestinal malignancies, including colon, gastric, rectal, and pancreatic tumors, 70% of lung cancers, about 50% of breast cancers and a majority of head and neck (HNC) cancers. For this reason, CEA has been a vaccine target in cancer immunotherapy studies for several decades. A variety of different vaccine platforms have been employed to target this antigen, including protein/ peptide, DNA, viral vector, dendritic cell, and exosome-based vaccines.
Historically, the goal of CEA-based vaccines has been to activate and expand CD8+ T cells against CEA-bearing cancer cells. Several CEA peptide epitopes have been identified and reported for their capacity to elicit a CD8+ T cell response in vitro. One of these peptides: the HLA-A*0201-restricted YLSGANLNL, corresponding to CEA571-579 (also known as CEA peptide-1 or CAP-1 peptide; in some publications, it is also referred to as CEA605-613 ), has been used in several clinical trials. It was initially identified in a clinical trial with a vaccinia virus-based CEA vaccine, Specific in vitro response to CAP-1 peptide was observed only with post-vaccination samples (Yang et. al.). Fong et. al. reported a phase I clinical trial administering autologous dendritic cells (DC) loaded with the CEA605-613, 610D (YLSGADLNL), the CAP-1 peptide containing an asparagine to aspartic acid (N to D) substitution to increase immunogenicity. After the vaccination regiment, two of 12 patients experienced dramatic tumor regression, one patient had a mixed response, and two had stable disease. Clinical response correlated with the expansion of CD8 tetramer+ T cells. Furthermore, only post-vaccinated but not pre-vaccinated lymphocytes showed specific in vitro cytotoxicity against SW403 tumor cells (HLA*A0201+, CEA+) and not against control target cells: SW1417 (HLA*A0201−, CEA+), or A375 (HLA*A0201+, CEA−).
Ignyte Bio’s CEA-specific CD8+ T cells were generated against the native CEA571-579 (YLSGANLNL) peptide. This peptide also known as CEA peptide-1 or CAP-1 and in some publications, it is termed CEA605-613.
Figure 1 shows specific recognition of the CEA571-579 (YLSGANLNL) in association with HLA-A-02:01 as shown by the tetramer binding study. Figure 2 shows specific IFN-γ secretion and specific lysis when HLA-A-02:01+ target cells were incubated with the CEA571-579 peptide but not the control HPV E711-20 (YMLDLQPETT) peptide.
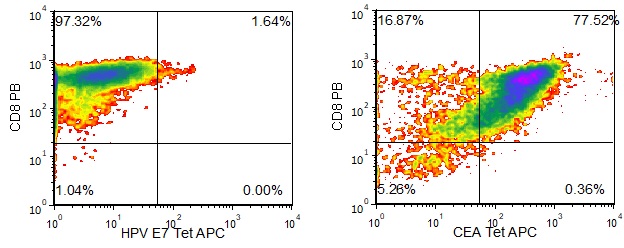
Figure 1. Recognition of Antigenic Peptide CEA571-579 Demonstrated by Peptide/MHC Tetramer Binding Analysis. Cryopreserved T cells were thawed and stained with APC-labelled HLA-A-02:01-CEA571-579(YLSGANLNL, CEA Tetramer APC) or a control tetramer HLA-A-02:01-HPV E711-20(YMLDLQPETT, HPV E7 Tetramer APC). These cells were counterstained with anti-CD8 Pacific Blue reagent and analyzed by flow cytometry. Non-viable cells were excluded from the analysis using 7-AAD.

Figure 2. Antigen-Specific IFN-γ Secretion and Cytotoxicity Data. Freshly thawed anti-CEA T cells were plated at 2 x 104 cells/well in the presence of 2 x 104 T2 cells, an HLA-A-02:01+ B-LCL (ATCC, Manassas, VA) and different concentrations of CEA571-579 (YLSGANLNL): CEA, or HPV E711-20 (YMLDLQPETT): HPV E7 control peptide in a 96-well round bottom plate. After 18-24 hours of incubation at 37oC, 5% CO2, culture supernatants were harvested and assayed for IFN-g using the Lumit™ IFN-γ Immunoassay (Promega, Madison, WI). IFN-γ concentration is plotted against CEA and control peptide concentrations (upper graph). Remaining cells in each well were stained with the viability dye 7-AAD and analyzed using flow cytometry. % Cytotoxicity (= % 7-AAD+ target cells) is plotted against the respective peptide concentrations (lower graph).
