Antigen-Specific T Cells to GAD65
Our scientists were among the first to develop custom antigen-specific T cells for research use and have created them against a diverse range of targets, including viral, tumor, and self-antigens.
We’re now developing the next generation of antigen-specific T cells (both CD4+ and CD8+) to target some of today’s most prevalent and challenging diseases. More on that below. But first, a primer on antigen-specific T cells.
The Role of Antigen-Specific T Cells in Disease Research and Treatment
T cells are a major player in the immune response in various diseases, including cancer and pathogenic infections, and are mediators in inflammation and autoimmunity. A large body of research has been conducted over the past few decades to manipulate T cell responses, leading to many clinical strategies including cancer vaccines, T cell adoptive therapy, CAR-T therapy, immune-oncology, and the use of regulatory T cells for autoimmune diseases.
Antigen-specific T cells are an important tool in T cell biology research and potency assays. Investigators can isolate them directly from the disease site (e.g., tumor-infiltrating lymphocytes (TIL) or inflammatory lesion infiltrate populations), but these procedures often yield a limited number of cells due to low cell frequency and lack of robust isolation methods.
Alternatively, antigen-specific T cells can be generated in vitro using antigen-presenting cells pulsed with whole antigens or peptides. However, this process is often time-consuming with a low success rate.
About Ignyte Bio’s Antigen-Specific T Cells
Ignyte Bio offers antigen-specific T cells for research use you can rely on.
- Typically generated using multiple in vitro stimulations with peptide antigens
- Not immortalized or genetically modified, so they more closely mimic physiological T cells
- Specificity analyzed using the cognate peptide/MHC tetramer binding as well as interferon-gamma (IFN-γ) and cytotoxicity assays for CD8 products, or antigen-specific proliferation assay for CD4 products
Announcing Ignyte Bio’s Newest Antigen-Specific T Cells : anti-GAD65 CD4+T Cells
Type 1 Diabetes (T1D) is the result of a progressive T cell-mediated autoimmune destruction of insulin-producing b cells in the pancreatic islets of Langerhans. Several b cell autoantigens have been implicated in the triggering of islet autoimmunity. The 65 kd isoform of glutamic acid decarboxylase (GAD65) is one of the major autoantigens in T1D. Autoreactive T cells can be detected in PBMC from T1D or at-risk subjects after a primary culture with several immunodominant GAD65 peptides, including: 274-286 and 555-567 (1).
Ignyte Bio’s GAD65-specific CD4+ T cells were generated against the GAD65274-286 (IAFTSEHSHFSLK) peptide.
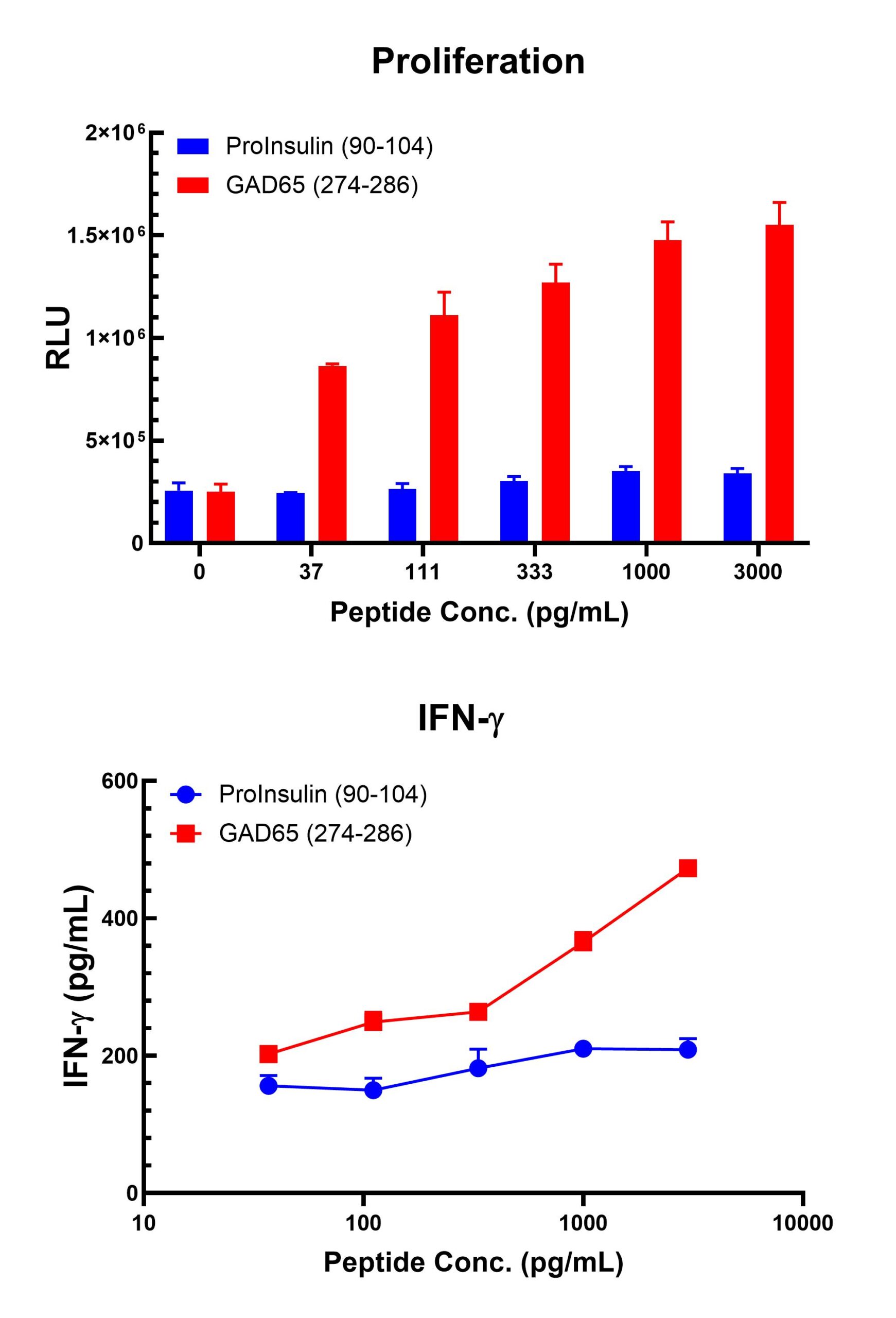
Figure 1. Antigen-Specific CD4 T Cell Proliferation and IFN-γ Data.
Freshly thawed anti-GAD65 T cells were plated at 2 x 104 cells/well in the presence of 2 x 104 mitomycin-C inactivated autologous B-LCL cells (HLA-DRB1*0401+) and different concentrations of GAD65274-286 (IAFTSEHSHFSLK): GAD65 (274-286), or Proinsulin90-104 (GIVEQCCTSICSLYQ) Proinsulin (90-104) control peptide in a 96-well round bottom plate. Each assay condition was conducted in triplicates. After 4 days of incubation at 37oC, 5% CO2, IFN-γ levels were measured from culture supernatant (IFN-γ Lumit assay, Promega, Madison, WI) and plotted versus the respective peptide concentrations (lower graph). The relative number of viable cells in each well were measured using the CellTiter Glo 2.0 (Promega, Madison, WI), a luminescent assay that quantitates the amount of ATP present. Relative Luminescence Unit (RLU) is plotted against the respective peptide concentrations (upper graph).
